Cysto-Lithotomy
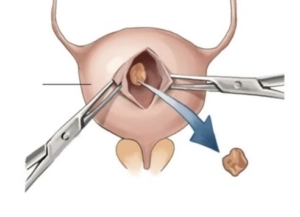
Open removal of a large bladder calculus
Why is it done?
- To break up a large bladder calculus (stone) that cannot be done endoscopically.
- It is done with open surgery (a cut above the pubic symphysis).
Risk factors causing this:
-
- Bladder outflow obstruction
- BPH with chronic retention.
- Urethral stricture.
- Neurogenic bladder.
- Renal calculi disease.
- Metabolic disorders.
- Malnutrition.
- Chronic infections.
- Foreign objects in bladder.
- Bladder outflow obstruction
How is it done?
 A General anesthetic will be given.
A General anesthetic will be given.- A sterile surgical field is prepared.
- Prophylactic antibiotics are given.
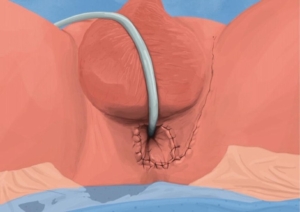
- An indwelling catheter is inserted, and the bladder is then distended with fluid (saline).
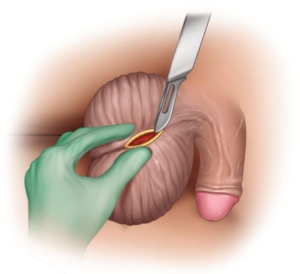
- A small lower abdominal incision is made, splitting the Linea alba and opening the distended bladder in the midline.
- The stone is removed through the whole with a grasping instrument.
- The bladder is inspected and then closed in 2 layers.
- Skin is closed.
- A catheter will be left for 2 weeks.
What to expect after the procedure?
- Hematuria (blood in your urine)
- You will have an indwelling catheter (IDC), which will remain in your bladder.
- You may have a continuous bladder irrigation with Saline to help clear the bleeding.
- When your urine is clear and your bowels are functioning, you will be discharged with catheter care instruction.
- You will have this indwelling catheter for 2 weeks.
- A cystogram will be arranged at approx. 14 days to exclude any urine leaks prior to removal of your catheter.
- If there are any urine leaks, your catheter will remain a further 7 days, or until the leak is sealed.
- Pain on initial passing of urine when the catheter is removed.
- Bladder infection ranging from a burning sensation to, fever, to puss (rare).
- Lower abdominal discomfort which will persist for a few days.
- NB! Each person is unique and for this reason symptoms vary.
What next?
- This all depends on what is found during the procedure. All the options will be discussed in detail.
- There may be some blood in the urine. This can be remedied by drinking plenty of fluids until it clears.
- Anatomical causes of the stones will be discussed and surgical options in treatment may be discussed
- Patients should schedule a follow-up appointment within 4-6 weeks to discuss the etiology of the calculus as well as what other procedures may be involved to prevent this from occurring again.
Download Information Sheet



 This procedure is performed under general anesthetic.
This procedure is performed under general anesthetic.
 This procedure is done under general anesthetic.
This procedure is done under general anesthetic.