Male reproductive health is an essential part of overall well-being, yet it is often overlooked or misunderstood. Understanding how the male reproductive system works, common health issues, and ways to maintain reproductive health can help men live healthier and more confident lives.
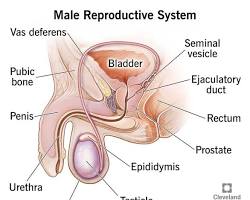
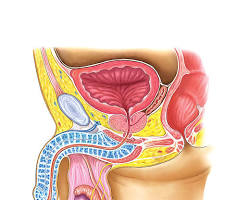
What Is the Male Reproductive System?
The male reproductive system is a group of organs responsible for producing, storing, and delivering sperm. It also produces male hormones, mainly testosterone, which play a vital role in physical development, fertility, and sexual function.
Main Organs of the Male Reproductive System
- Testes (Testicles): Produce sperm and testosterone
- Scrotum: Holds and protects the testes
- Epididymis: Stores and matures sperm
- Vas Deferens: Transports sperm
- Seminal Vesicles & Prostate Gland: Produce seminal fluid
- Penis: Delivers semen during ejaculation
Functions of the Male Reproductive System
The primary functions include:
- Sperm production (spermatogenesis)
- Hormone production (testosterone)
- Sexual function and reproduction
- Ejaculation and fertility
Testosterone also affects muscle mass, bone density, voice depth, mood, and libido.
Common Male Reproductive Health Problems
1. Erectile Dysfunction (ED)
Erectile dysfunction is the inability to achieve or maintain an erection. It can be caused by stress, anxiety, diabetes, heart disease, or hormonal imbalance.
2. Low Testosterone Levels
Low testosterone may cause fatigue, low sex drive, depression, and reduced muscle mass. Aging, obesity, and certain medical conditions are common causes.
3. Infertility
Male infertility often results from low sperm count, poor sperm quality, or blocked reproductive ducts. Lifestyle factors such as smoking and excessive alcohol intake also contribute.
4. Prostate Problems
- Prostatitis (inflammation)
- Benign Prostatic Hyperplasia (BPH)
- Prostate cancer
Regular check-ups help detect prostate issues early.
5. Testicular Disorders
- Testicular cancer
- Testicular torsion
- Varicocele
Early detection through self-examination is crucial.
Tips to Maintain Male Reproductive Health
Maintaining male reproductive health is essential for fertility, hormone balance, sexual performance, and overall quality of life. Whether you are experiencing symptoms or simply want to stay proactive, following these evidence-based tips can help reduce the risk of reproductive health problems and support long-term wellness.
Men in Australia, especially those seeking care from a urologist Brisbane (also commonly searched as eurologist Brisbane), are encouraged to prioritize prevention and early medical consultation.
1. Maintain a Healthy Lifestyle
A healthy lifestyle directly affects testosterone levels, sperm quality, and blood circulation.
- Eat a balanced diet rich in fruits, vegetables, whole grains, healthy fats, and lean protein such as fish, chicken, eggs, and legumes
- Include foods high in zinc, omega-3 fatty acids, and antioxidants to support sperm health
- Exercise regularly to improve cardiovascular health and hormone regulation
- Maintain a healthy weight, as obesity is linked to low testosterone and reduced fertility
2. Avoid Harmful Habits
Certain habits can significantly harm male reproductive function.
- Quit smoking, as tobacco reduces sperm count, damages sperm DNA, and increases erectile dysfunction risk
- Limit alcohol consumption, since excessive drinking can lower testosterone levels and impair sexual performance
- Avoid illegal drug use, including anabolic steroids, which can disrupt hormone production and fertility
3. Manage Stress Effectively
Chronic stress increases cortisol levels, which can interfere with testosterone production and sexual desire.
- Practice relaxation techniques such as meditation, deep breathing, or mindfulness
- Engage in regular physical activity to reduce stress naturally
- Ensure adequate sleep, as poor sleep is associated with hormonal imbalance
If stress-related symptoms persist, a consultation with a urologist Brisbane (also commonly searched as eurologist Brisbane) or healthcare professional may be recommended.
4. Practice Safe Sex
Safe sexual practices are crucial for protecting reproductive health.
- Use condoms to reduce the risk of sexually transmitted infections (STIs)
- Untreated STIs can cause inflammation, scarring, and fertility issues
- Regular sexual health screenings are advised, especially for sexually active individuals
5. Get Regular Medical Check-ups
Routine medical evaluations help detect reproductive issues early, before complications develop.
- Schedule regular health check-ups and blood tests to monitor hormone levels
- Men over 40 should discuss prostate health screenings with a doctor
- A urologist Brisbane (also commonly searched as eurologist Brisbane) specializes in male reproductive health, urinary conditions, fertility issues, erectile dysfunction, and prostate disorders
When to See a Doctor
Early medical consultation improves treatment success and long-term outcomes. You should seek advice from a doctor or urologist Brisbane (also commonly searched as eurologist Brisbane) if you experience:
- Persistent erectile dysfunction or difficulty maintaining an erection
- Pain, swelling, lumps, or discomfort in the testicles
- Difficulty conceiving after 12 months of trying
- Low libido, fatigue, mood changes, or other symptoms of hormonal imbalance
- Urinary problems such as weak stream, frequent urination, or pain
Seeing a qualified urologist Brisbane (also commonly searched as eurologist Brisbane) allows for accurate diagnosis, personalized treatment, and professional guidance on maintaining optimal male reproductive health.
Frequently Asked Questions (FAQs)
Is male reproductive health affected by age?
Yes. Testosterone levels and sperm quality may decline with age, but healthy lifestyle choices can slow the effects.
Can diet improve male fertility?
Yes. Foods rich in zinc, omega-3 fatty acids, and antioxidants support sperm health.
How often should men check their reproductive health?
Men should perform monthly testicular self-exams and visit a doctor annually or as recommended.
Book Your Appointment Today
If you’re in need of a urologist in Brisbane, Dr. Jo Schoeman is here to help. With a commitment to patient-centered care and advanced treatment options, Dr. Schoeman is dedicated to improving the lives of her patients. Contact our office today to schedule a consultation and take the first step toward better urological health.
Dr Jo Schoeman, Urologist
Suite 46, Level 4
The Wesley Medical Centre
Wesley Hospital
Auchenflower Brisbane