Pelvi-Ureteric Junction Repair (PUJ) – Robotic Assisted
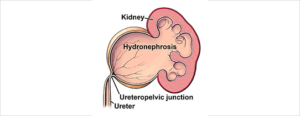
A congenital or acquired narrowing in the ureteric pelvis junction. This narrowing is excised with a reconnection. There are several techniques described in repairing this: I prefer the Dismembered Pyeloplasty
Why is it done?
- High grade obstruction.
- Causing deterioration of renal function.
- Thinning of renal cortex.
- Chronic pain.
- Chronic infection.
- Recurrent renal calculi.
Causes
- Congenital lack of muscle, or neuro transmission in this area, causing a non-functioning part leading to obstruction.
- Vesico-ureteric reflux, longstanding can also cause this.
- Usually diagnosed in kids.
- Crossing vessel.
How is it done?
Robotic assisted pyeloplasty.
- Types
-
- Dismembered.
- Foley’s Y-V Pyeloplasty.
- Culp-Dewierd.
- Pelvi-calyceal pyeloplasty.
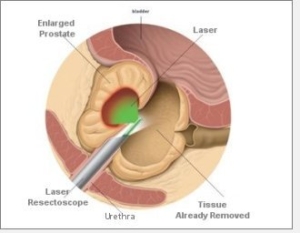
- Endopyelotomy with laser.
- Patients will receive a general anaesthesia.
- Prophylactic antibiotics is given.
- The correct ureteric system is identified and marked while you are awake.
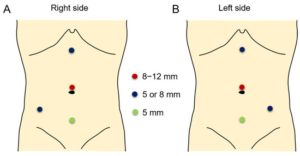
- This will be mostly a robotic / laparoscopic procedure.
- The endoscopic procedure is reserved as a second line in my practice.
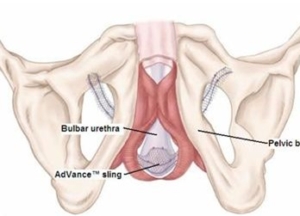
- Laparoscopic ports are placed
- The affected ureter is exposed, the defect cut out with a re-anastomosis of a spatulated ureter to a trimmed renal pelvis over a ureteric stent.
- An indwelling catheter is placed. A drain is placed.
-
What next?
- You may be in hospital for 3 days
- Your drain will be removed when there is no urine draining.
- Your catheter will be removed the following day.
- As soon as you are comfortable with no signs of pain and emptying your bladder sufficiently, you will be discharged
- A ward prescription may be issued on your discharge, for your own collection at any pharmacy.
- A follow-up appointment will be scheduled for 6 weeks to remove your ureteric stent under local anaesthesia with a Flexible Cystoscope.
- A review with a CT IVP will be scheduled 6 weeks after this to check on the end result of the ureter.
- Any pain or signs of fever require an urgent review.
- DON’T SUFFER IN SILENCE, OR YOU WILL SUFFER ALONE!
Possible Complications
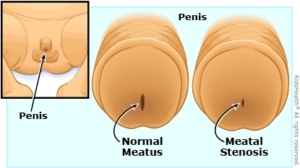
- Re-stenosis with recurrent obstruction.
- Second procedure.
- With further deterioration of renal function, you may require a nephrectomy where affected kidney contributes < 15-20% of total renal function.
- Urine leak, Urinoma, requiring drainage.
- Infection possible sepsis requiring long-term antibiotics.
Download Information Sheet




 Your urine output will be measured each time you urinate, and the residual will be measured. (Patients will be required to do this up to 3 times.)
Your urine output will be measured each time you urinate, and the residual will be measured. (Patients will be required to do this up to 3 times.)